Bio-Digital AI: Can AI Merge with Biology by 2026


Introduction: The Dawn of Bio-Digital Convergence
Bio-digital AI represents the next major leap in human innovation, a space where artificial intelligence begins to merge with biology itself. What was once the realm of science fiction is now a rapidly evolving reality, visible in brain–computer interfaces (BCIs) that translate thoughts into digital commands, AI-powered wearables that predict illnesses before symptoms appear, and synthetic biology driven by machine learning to design new forms of life. This convergence marks a turning point in how we understand health, longevity, and human capability.
By 2026, these technologies will no longer be confined to research labs. Neural implants are enabling patients to regain lost mobility and speech, AI-based drug discovery is cutting development timelines by over 60 percent, and digital twins built on biological data are making personalized healthcare a practical reality. The shift is profound as medicine is moving from reactive treatment to predictive prevention, where biological signals and digital intelligence continuously interact to keep us healthier and extend human life.
Yet, this integration also forces us to confront complex ethical and social questions. Who controls neural data when technology can interpret brain activity? How should societies govern enhancement technologies that increasingly blur the line between healing and human upgrade? As bio-digital innovation accelerates, the question remains whether it will serve as a force for shared progress or widen the divide between those who benefit and those left behind. Ultimately, the future of this convergence will hinge less on what we create and more on how thoughtfully and ethically we choose to shape it.
In this blog, we will dissect the rise of bio-digital AI, exploring the breakthroughs driving it, the opportunities it creates across medicine and biotechnology, the risks it poses to ethics and privacy, and the regulatory and societal frameworks needed to manage this transformation responsibly. The fusion of AI and human biology is already underway; what remains to be seen is whether we can shape it in a way that enhances both technology and humanity.
The Current State: Where Biology Meets Silicon
The convergence of AI and biology is no longer confined to theoretical research. The technologies that connect neurons, decode DNA, and read biometric signals are rapidly advancing into clinical and consumer use.

Neural Interfaces Breaking New Ground
Brain–computer interfaces have progressed from laboratory curiosities to functioning human implants. Reports highlighted by Nature show that Neuralink successfully implanted its wireless interface in at least three human patients by late 2024, with 20 to 30 additional procedures planned for 2025. The first recipient was able to control a computer cursor, play video games, and even post online, all using neural activity alone.
Neuralink may have drawn the most attention, but it is far from the only player shaping the brain–computer interface landscape. Several companies, including Synchron, Precision Neuroscience, Paradromics, and Blackrock Neurotech, are making significant progress in developing technologies that help patients regain communication and mobility. As highlighted by BuiltIn, these firms are advancing a new generation of BCIs using different methods and levels of invasiveness. Synchron’s “stentrode,” for instance, is inserted through blood vessels rather than open-brain surgery, offering a safer and less invasive pathway to connect the brain with digital systems. Despite their varied approaches, they all share one mission: restoring lost function and improving quality of life through direct communication between the brain and machines.
Wearable Sensors and the Rise of Bio-Data Analytics
Wearable health technology is rapidly evolving beyond its early role as a step counter or sleep tracker. Today’s AI-powered devices are becoming intelligent health companions capable of predicting potential risks before they arise. Industry insights from Grand View Research estimate that the global wearable medical device market stands at around $42.7 billion in 2024 and is projected to grow to $54 billion by 2025, reflecting this accelerating shift.
Modern wearables now integrate multiple sensors with AI-driven analytics to track everything from glucose and blood pressure to stress levels in real time. As highlighted by Forbes Health, the next wave of innovation lies in continuous contextual analysis, where these devices not only gather data but also interpret it based on the user’s environment and behavior.
This evolution marks a major shift in healthcare, from reactive treatment to proactive prevention, enabling individuals to address potential health issues long before symptoms appear.
AI-Bio Data Integration in Action
The convergence of biological and digital data is creating an entirely new model of healthcare. Predictive models now analyze continuous streams of bio-signals to detect irregularities long before they manifest. For instance, systems trained on temperature and heart-rate variability can forecast hormonal shifts or stress responses.
By turning every user into a real-time data generator, these devices enable clinicians to identify patterns that are invisible to conventional diagnostics. The impact reaches beyond wellness where it’s creating a blueprint for preventive medicine at scale.
Potential by 2026: The Converging Landscape
As 2026 nears, the convergence of biology and artificial intelligence is accelerating from concept to commercial and clinical reality. Neural interfaces, AI-enhanced biotechnology, and digital-twin models are forming an interconnected ecosystem where biology and computation begin to operate as one.
AI-Interpreted Neural Signals
Recent findings from Nature Machine Intelligence confirm that today’s neural systems already allow paralyzed patients to operate computers using thought alone. The next milestone is closed-loop communication, where BCIs send feedback, like touch or pressure, back to the brain. Neuralink’s current experiments focus precisely on this, attempting to recreate natural sensation alongside movement.
This could redefine prosthetics and physical therapy, allowing patients not just to act but to feel through digital extensions of their own nervous systems. If successful, this two-way communication between mind and machine could eventually make artificial limbs and assistive devices indistinguishable from natural movement.
Synthetic Biology Meets Machine Learning
The collaboration between synthetic biology and AI is arguably the most transformative development of this decade. It is reshaping how we design living systems and accelerating research from hypothesis to implementation.
The integration is visible across four major fronts:
- Accelerating Innovation: AI now powers the design of genetic sequences and proteins. Platforms like DeepMind’s AlphaFold have solved complex protein-folding problems, enabling rapid discovery of new enzymes and therapeutic molecules.
- Expanding Impact Across Sectors: The applications of synthetic biology extend from healthcare to agriculture and environmental sustainability. With AI’s ability to optimize large datasets, progress toward a bio-based economy is expected to accelerate through the next decade.
- Smarter Experimentation: Laboratory automation, guided by machine learning, reduces both error and cost. AI-controlled systems now conduct experiments and analyze results continuously, cutting development cycles from years to weeks.
- Revolutionary Tools: Companies such as Insilico Medicine, Profluent, and Deep Chain use generative AI to design novel compounds, while BioAge Labs focuses on anti-aging therapies by linking AI analysis with biological data.
Collectively, these advances are redefining biology as a programmable system, transforming the laboratory into an information-driven environment for innovation.
Opportunities: The Promise of Bio-Digital Convergence

The Healthcare Revolution
The most immediate and tangible effects of bio-digital AI are emerging in healthcare. BCIs now allow individuals with paralysis to regain movement and communication, while AI-driven prosthetics respond dynamically to brain activity. Neuralink and Precision Neuroscience are both refining systems that translate neural signals into speech and physical control, marking a new era of assistive medicine.
Wearable AI systems are also evolving rapidly. Predictive algorithms can now identify arrhythmias before they become dangerous, detect early signs of chronic stress, and even forecast labor onset with precision. This marks a transition from reactive treatment to predictive and preventive medicine.
For hospitals and insurers, these tools offer not only improved patient outcomes but also significant cost reduction through early intervention. As McKinsey HealthTech Insights outlines, predictive care could reduce long-term healthcare costs by up to 15 percent globally by 2030.
Human Augmentation and Longevity
Beyond medical treatment, bio-digital AI is opening possibilities for enhancement and longevity. AI systems are accelerating biomarker discovery, helping scientists understand aging at the cellular level. This knowledge enables doctors to design personalized prevention and treatment plans tailored to each patient’s unique biology.
Drug discovery is also being revolutionized. MIT Technology Review reports that AI-based molecular modeling has shortened the pre-clinical phase of drug discovery by more than 60 percent. Companies such as BioAge Labs and Insilico Medicine are utilizing AI to identify therapies that target the root causes of aging, including cellular inflammation, mitochondrial decline, and DNA damage.
By 2026, AI-designed molecules and proteins are expected to enter human clinical trials, marking the first generation of drugs developed through human-machine collaboration.
Personalization at Scale
Personalization is emerging as the defining feature of bio-digital healthcare. Integration between AI wearables, hospital records, and genomic data enables systems to adapt to each user in real time. Every data point, from heart rate to hormonal rhythm, becomes a feedback signal in a continuous health loop.
This model transforms care from one-size-fits-all to constantly optimized. The result is medicine that evolves daily, based on individual biology, environment, and behavior.
Challenges and Risks: The Dark Side of Convergence
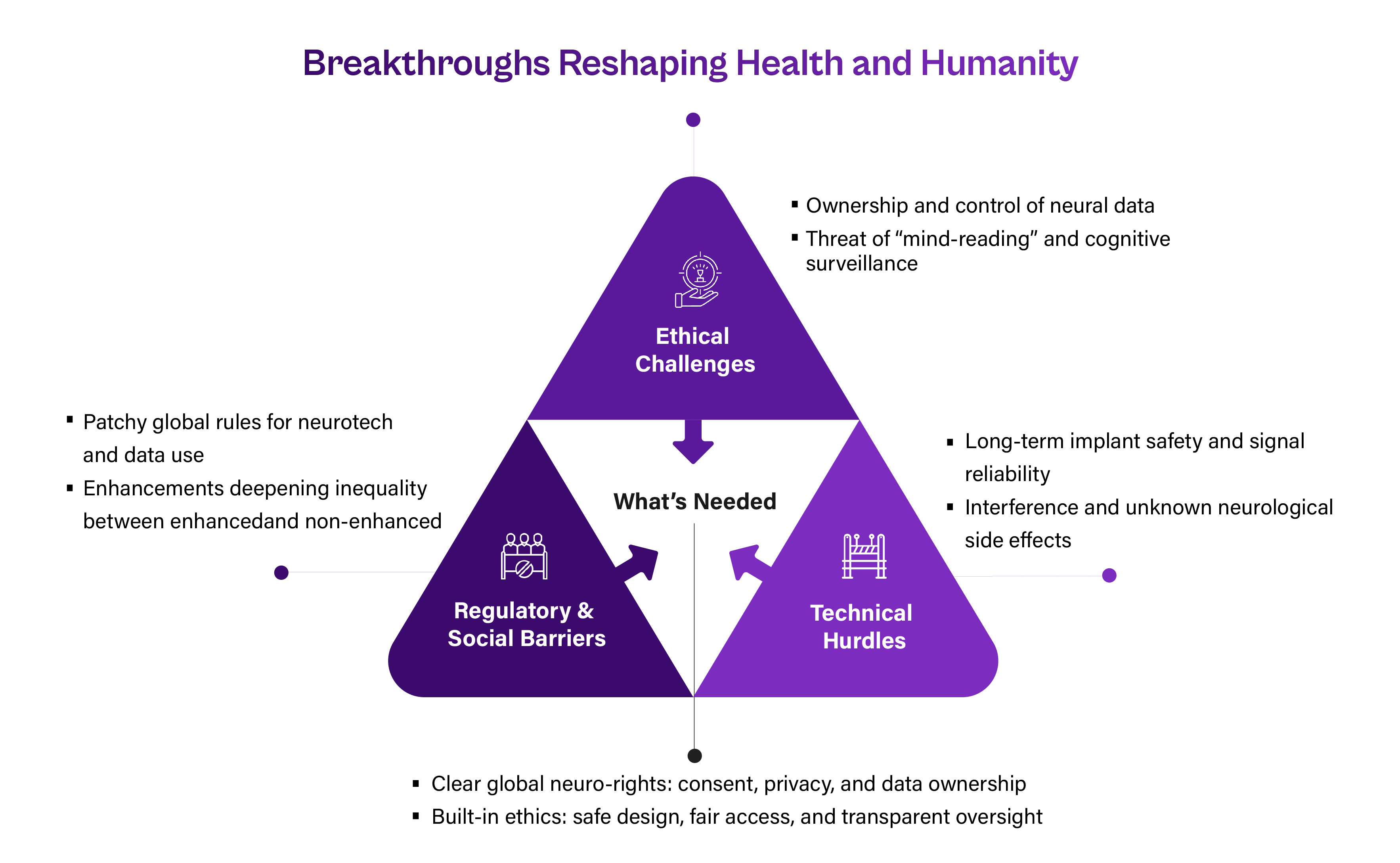
Ethical Landmines: Autonomy and Identity
As AI begins interacting directly with human cognition, questions about autonomy and privacy intensify. If neural interfaces can capture or interpret brain signals, who controls that data? If AI systems influence bodily functions, where does personal agency begin and end?
Bioethicists warn of potential “cognitive transparency”, a world where thoughts could, in theory, be observed or predicted. Frontiers in Neuroscience emphasizes the need for “neuro-rights” frameworks to ensure privacy, consent, and ownership of brain data. Without such safeguards, trust could erode quickly.
Moreover, vulnerable participants may feel pressured into trials due to hype or miscommunication about capabilities. Informed consent must remain at the center of every bio-digital experiment.
Technical Hurdles: Integration Complexity
Despite its promise, bio-digital AI still faces significant engineering challenges.
- Durability: Neural implants must remain safe and functional for years without degradation. Some early devices, including Neuralink prototypes, have encountered thread retraction issues, highlighting the delicate balance between flexibility and reliability.
- Signal Quality: Brain signals are inherently noisy. Achieving accurate, real-time interpretation remains a technical bottleneck, requiring constant refinement of AI decoding algorithms.
- Interference Risks: Electromagnetic interference with other medical devices can disrupt function or generate excess heat, raising safety concerns.
- Unknown Long-Term Effects: The neurological and psychological impacts of long-term implant use remain uncharted, demanding continuous study before widespread deployment.
Regulatory Complexities
The regulatory environment is advancing but remains fragmented. There is no unified framework governing privacy and data ownership for brain–computer interfaces. Without standardization, companies may hold unprecedented access to sensitive neural data without sufficient oversight.
A notable milestone came in 2025 when Precision Neuroscience’s Layer 7 cortical interface became the first next-generation wireless BCI to receive full FDA clearance. Yet, approval standards differ significantly across jurisdictions. Some classify BCIs as medical devices; others view them as enhancement technologies, creating legal ambiguity.
Policy analysts across argue that global coordination is critical. Otherwise, innovation will continue to outpace regulation, leaving ethical and safety concerns to lag.
The Inequality Amplifier
Bio-digital AI could become the ultimate engine of inequality. Longevity and enhancement technologies are expensive, and their initial benefits may accrue only to those with resources. The World Economic Forum estimates the economic cost of age-related chronic diseases will reach $47 trillion by 2030, underscoring both the need for innovation and the risk of unequal access.
Without deliberate intervention, we risk a two-tier society: one optimized by AI-driven biology, the other dependent on conventional healthcare. Addressing equity early is essential for sustainability.
Technologies to Watch: The Building Blocks of the Bio-Digital Future
Next-Generation Neuro-Interfaces
The next wave of brain–computer interfaces is defined by adaptability, precision, and clinical safety.
- Precision Neuroscience: Its Layer 7 interface, approximately one-fifth the thickness of a human hair, features 1,024 electrodes and conforms seamlessly to brain tissue, enabling high-resolution signal capture.
- Synchron: Its minimally invasive “stentrode” technology travels through blood vessels rather than open surgery, making it a safer alternative for many patients.
- Medtronic: Its BrainSense adaptive stimulation system utilizes neural feedback to adjust therapy, tailoring treatment in real-time dynamically.
Together, these companies represent a new phase in neuro-interface development, less invasive, more intelligent, and designed for clinical scalability.
Synthetic Biology + AI Synergy
Synthetic biology is rapidly becoming AI’s most powerful laboratory partner. The field is shifting from hypothesis-driven to algorithm-driven innovation.
- AI automates DNA synthesis and protein design, enhancing speed and reproducibility.
- Firms like Profluent and Deep Chain are applying generative AI to create entirely new enzymes and peptides.
- Insilico Medicine recently initiated human trials for a drug entirely designed by AI, a world first in pharmaceutical R&D.
- BioAge Labs continues to integrate AI with biological aging data to identify longevity therapies.
This collaboration shortens R&D cycles and reduces error margins, helping life-science companies commercialize discoveries faster than traditional methods.
Digital Twins and Predictive Models
AI’s predictive modeling capability is now enabling digital twins, virtual biological replicas of individuals that simulate health outcomes.
- “Aging clocks,” built on genomic and metabolic data, estimate biological rather than chronological age.
- Companies like TruDiagnostic and GlycanAge are pioneering these models, allowing clinicians to forecast disease risk years in advance.
- According to Harvard Health Publishing, digital twin technology could soon underpin personalized therapy design, thereby improving the accuracy of preventive care and treatment planning.
Beyond 2026: What Lies Ahead
The merger of AI and biology will continue, but several breakthroughs will still be beyond reach by 2026.
- Limited Adoption of Neural Implants: BCIs will remain primarily in clinical trials or specialized medical applications, not mass consumer markets.
- Experimental AI–Biology Fusion: A truly symbiotic integration of digital and biological intelligence will stay experimental, constrained by technical complexity and ethical oversight.
- Ongoing Ethical and Regulatory Challenges: Debates over consent, identity, and ownership will persist as governments and companies navigate uncharted territory.
- Cost and Accessibility Barriers: Enhancement technologies will likely remain expensive and localized, thereby limiting their global reach.
- Incomplete Understanding of Long-Term Effects: More longitudinal data will be required before large-scale integration into everyday healthcare.
Still, Frontiers in Cellular Neuroscience emphasizes, the integration of AI and synthetic biology is growing rapidly, setting the stage for a bio-based society within the next few decades.
Preparing for the Bio-Digital Future
Building a responsible bio-digital ecosystem will require cooperation across sectors.
- Regulators must update frameworks to capture convergence-related risks through harmonized data governance and device classification policies.
- Healthcare Systems should invest in digital infrastructure, training, and equitable access initiatives to safely integrate emerging technologies.
- Technologists must embed transparency, data security, and ethical considerations from the design stage to build user trust.
- Society must engage in open dialogue about how far humanity should go in merging with machines, striking a balance between innovation and identity.
Conclusion: Readiness, Caution, and the Long Game
So, will AI merge with our biology by 2026? Only partially. We will see dozens of patients with functional neural implants, millions wearing AI-powered devices, and the first AI-designed drugs entering human trials. Regulators will begin to catch up, and the conversation about ethics, identity, and equality will grow louder.
Yet full biological integration where AI becomes an active and internal component of human life will take longer. It will demand not just technical achievement but social consensus and legal clarity.
The decade from 2025 to 2035 will mark the culmination of this transformation. Neural interfaces may become as common as pacemakers, AI health monitoring as routine as smartphones, and synthetic biology as critical as software development once was.
Bio-digital AI holds enormous promise, with the potential to help us heal faster, live longer, and even push the limits of what our bodies can achieve. Turning that potential into reality will take more than innovation; it will require foresight, effective regulation, and a strong commitment to keeping human values at the center. This merger of intelligence and biology is not happening in one big leap but through gradual steps that are already reshaping how we live, think, and define what it means to be human in a connected world.
Future-Proof Your Enterprise with Cogent Infotech
AI, automation, and digital intelligence are redefining workflows and workforce capabilities. Our teams help you modernize systems, optimize operations, and stay ahead of emerging technology shifts.
Your next competitive advantage starts here.







%402x.svg)


.jpg)

